Vol 3, No 3 (2025): Current Issue (Volume 3, Issue 3), 2025
Editorial
From Resource-Limited to Research-Rich: Unlocking the Scientific Potential of Developing Nations
Zuhair Dahham Hammood
For too long, the scientific narrative has been dominated by voices from wealthier nations. While their contributions are invaluable, the imbalance has left a vast reservoir of untapped knowledge and innovation in the developing world. Today, the time has come to shift the paradigm—from viewing developing countries as mere recipients of scientific progress to recognizing them as active producers of valuable, context-specific knowledge.
From Resource-Limited to Research-Rich is not a rhetorical flourish—it is a vision, a goal, and a challenge. It reflects a belief that scientific excellence is not the exclusive property of nations with abundant financial resources, but rather, a pursuit driven by curiosity, commitment, and community.
Developing countries, despite limited infrastructure and funding, are home to some of the most pressing health challenges—from endemic infectious diseases and rising non-communicable burdens to unique environmental and sociopolitical contexts. These challenges demand local insight, homegrown data, and context-sensitive solutions. The answers will not come from imported models alone. They must arise from within [1].
In this transformation, medical journals have a profound responsibility—not just as gatekeepers of knowledge, but as platforms for empowerment. Barw Medical Journal stands committed to this mission: to provide a voice to researchers working under constraints, to mentor and guide early-career scientists, and to uphold the integrity and quality of regional scholarship.
Success stories are already emerging. Across Africa, Asia, the Middle East, and Latin America, we are witnessing a rise in high-quality research led by local scientists. These efforts, often fueled by personal passion more than institutional support, prove that scientific ingenuity thrives even where resources are scarce [2].
However, more must be done. Governments must prioritize funding for health research. International agencies must listen more and dictate less. And academic partnerships must be based on equity, not extraction.
The path from resource-limited to research-rich is not paved overnight. It requires intentional investment, strategic collaboration, and relentless belief in the intellectual power of every nation. As we look ahead, let us remember: the next breakthrough in global health may very well come from a modest lab, in a hospital like ours, led by minds that simply needed a chance to be heard.
At Barw Medical Journal, we are here to amplify those voices.
Original Articles

The Effect of Clinical Knee Measurement in Children with Genu Varus
Kamal Jamil, Chong YT, Ahmad Fazly Abd Rasid, Abdul Halim Abdul Rashid, Lawand Ahmed
Abstract
Introduction
Children with genu varus needs frequent assessment and follow up that may need several radiographies. This study investigates the effectiveness of the clinical assessment of genu varus in comparison to the radiological assessment.
Methods
In this study, relationship between clinical and radiographic assessments of genu varus (bow leg) in children, focusing on the use of intercondylar distance (ICD) and clinical tibiofemoral angle (cTFA) as clinical measures, compared to the mechanical tibiofemoral angle (mTFA) obtained via scanogram, the radiographic gold standard for assessing lower limb deformity. Clinical measurements (ICD and cTFA) were gathered along with the mTFA from scanogram radiographs. Reliability was tested between two observers, and Spearman’s correlation coefficient was used to evaluate the relationships between the clinical and radiographic measurements.
Results
The study involved 36 children with an average age of 6.3 years. There were strong intra-rater reliability for both observers (ICC 0.87 for observer 1, ICC 0.97 for observer 2) and excellent inter-observer agreement (ICC 0.97). Positive correlations were found between cTFA and mTFA (r² = 0.67, p < 0.001), between ICD and cTFA (r² = 0.53, p < 0.001), and between ICD and mTFA (r² = 0.62, p < 0.001).
Conclusion
This study suupports the idea that clinical methods may be sufficient for evaluation, minimizing the need for radiation exposure and offering a reliable alternative to radiography.
Introduction
Genu varus, also known as bow-leggedness is defined as any separation of the medial surfaces of the knees when the medial malleoli are in contact, and the patient is standing in the anatomical position [1]. The prevalence of genu varus ranges from 11.4% to 14.5% [2,3]. It is found to be more prevalent in boys than in girls [2]. Genu varus may be physiological or pathological. There are multiple ways to aid in the screening and diagnosis of genu varus, which include clinical and radiological methods. Clinical methods such as intercondylar distance (ICD) and tibiofemoral angle measurement have been used to screen and assess the degree of genu varus. However, imaging modality such as a long-leg AP radiograph or scanogram is considered the gold standard assessment for lower limb deformity.
Many studies on genu varus in children have utilized either the clinical or radiological lower limb measurements to describe the tibiofemoral angle progression in normal children, data of normal ranges of knee angle in relation to age, and transition time from varus to valgus of different populations and ethnic groups [4-10].In a recent systematic review, it is proposed that children above the age of 18 months with genu varus should be closely monitored clinically using ICD or cTFA, whereby an ICD of more than 4 cm needed to be investigated for pathologic cause [11]. However, reliability has not been confirmed.
Hence, serial assessment might be needed to manage children with genu varus. Clinical methods of assessment are preferrable due to no exposure to radiation as compared to a radiograph but may be inaccurate or unreliable [12]. We are interested to find out the correlation between the radiological and clinical assessments.
Methods
Study design and setting
This was a single center cohort study. The study was conducted in an orthopaedic clinic of a tertiary hospital. Children with age ranging from 1 to 17 years old who were diagnosed as genu varus by orthopaedic specialists and has long leg radiograph done, were included. We excluded children who have previous history of fracture of the lower limb, had any knee swelling, tumour or contracture. Consent was taken from the parents before enrolment to the study. This study was conducted in accordance with the Declaration of Helsinki and was approved by the Universiti Kebangsaan Malaysia Institutional Ethical Committee (JEP-2020-194).
Procedure
The baseline data such as age, gender, weight/height and underlying diagnosis were taken. The knee intercondylar distance was measured using a measuring tape, with the child standing, and both medial malleoli touching. The centre of the medial femoral condyles was identified by palpation of the most prominent part of the distal femur. The measurement between the condyles was performed following the method described by Heath et al [13]. The reading was measured in centimetres as the intercondylar distance. The clinical tibiofemoral angle (cTFA) was measured with a goniometer, following the method described by Arazi et al [14]. With the child in standing, the anterior superior iliac spine, centre of the patella, and midpoint of the ankle joint were marked with a pen. After the marking of the tibiofemoral axis, the angle was measured and recorded. The angle was expressed in degrees. Illustrates the method of measurements on a patient (Figure 1).

A standardized long-leg anterior-posterior radiograph (scanogram) of lower limbs was obtained from hospital radiological database. The angle formed between the mechanical axis of the femur and the mechanical axis of tibia was recorded as mechanical tibiofemoral angle (mTFA). The mTFA was determined from digital X-Ray by using the measuring tool from Medweb (Medweb, Inc, San Francisco, CA) software. In bilateral cases, the limb with the worst angle measured was chosen for analysis.
The clinical and radiological measurements were performed by a single researcher (CYT), who was trained on the measurement technique. For the radiographic measurements, a prior intra- and inter-observer reliability study was performed on 10 radiographs by two main researchers (CYT and KJ) on the same children at two different intervals.
Data analysis
The intra- and inter-observer reliability of tibiofemoral angle measurement was measured using with 95% confidence intervals to gauge the precisions of the ICCs [15]. Correlations between clinical tibiofemoral angle (cTFA), mechanical tibiofemoral angle (mTFA) and intercondylar distance (ICD) were tested using Spearman’s Correlation test. Differences between cTFA and mTFA were investigated using paired sample t-test and Bland Altman 95% limits of agreement. All statistical analysis was performed using SPSS (v24, IBM, NY, USA). Statistical significance was set at a cut-off of p<0.05.
Results
There were 36 children included with the mean age of 6.3 years. Thirty-two were Malay (88.8%), while the remaining participants were three Indians (8.3 %) and one Chinese (2.7%) by ethnicity. Twenty-two children were male (61%) and 14 female (38%). There were five unilateral and 31 bilateral genu varus. Eleven children had Blount disease; 13 cases had rickets while the remaining 12 was managed as physiological genu varus.
Reliability study performed between two observers for the tibiofemoral angle measurements revealed Good intra-rater reliability for observer 1 (ICC 0.87) and Excellent intra-rater reliability for observer 2 (ICC 0.97). Excellent inter-observer agreement (ICC 0.97) was also shown.
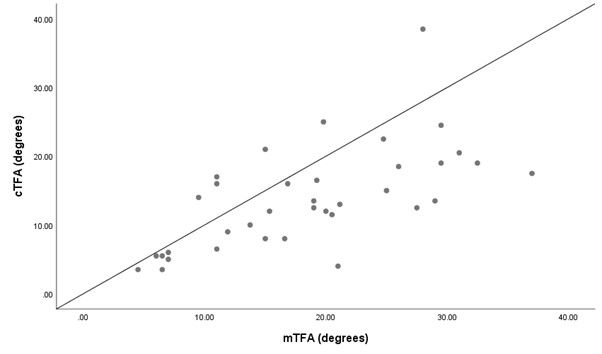
All thirty-six children (mean age 6.6 ± 5.7) were examined in standing position. The association between the radiological mTFA and clinical TFA measurements was assessed. Our findings revealed that there was a moderate correlation between cTFA and mTFA (r2=0.67, p< 0.001) (Figure 2).
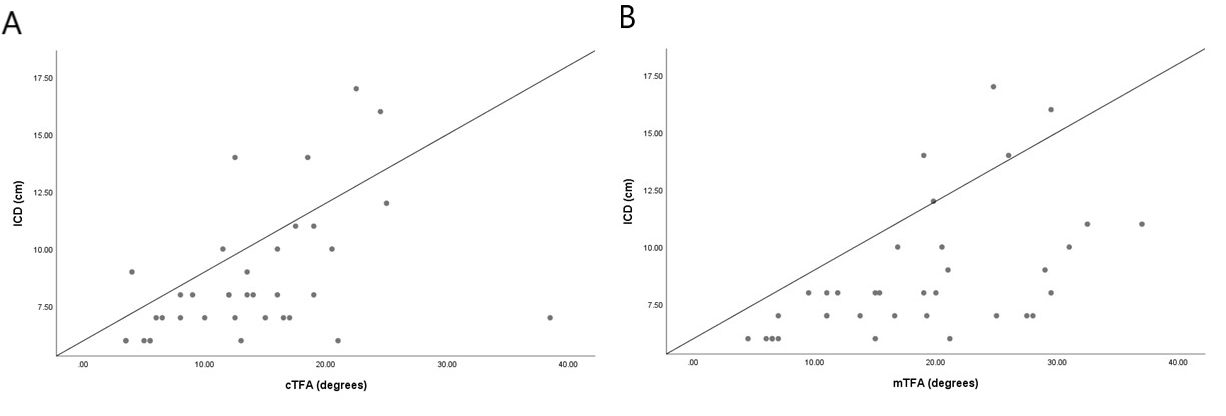
Subsequently, the association between the ICD and clinical TFA and between ICD and radiological mTFA measurements were assessed. We also found a moderate positive correlation between ICD and cTFA, (r2=0.53, p< 0.001) and between ICD and mTFA, (r2=0.62, p< 0.001), respectively (Figure 3).
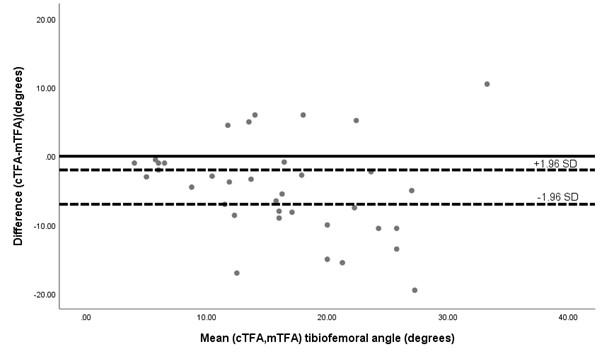
Paired t- test revealed a mean difference of -4.67 degrees between the cTFA and mTFA. The difference was statistically significant of p= 0.00. The limits of agreement revealed were a lower limit of -7.02 degrees and an upper limit of -2.34 degrees (Figure 4).
Discussion
We examined the correlation between clinical and radiographic TFA measurements of the lower extremities in 36 children with genu varus who has been referred to our centre. We found a significant correlation between radiological mTFA and clinical TFA. This result is in parallel with other studies by [16,17]. Navali et al concluded that goniometer measurement appears to be valid alternatives to the mechanical axis on full-leg radiograph for determining frontal plane knee alignment [17]. Kraus et al also concluded knee alignment assessed clinically by goniometer or measured on a knee radiograph is correlated with the angle measured on the full-limb radiograph [17]. However, both studies were carried out in adults’ population with osteoarthritis knee. Our study determined the correlation between radiological and clinical TFA specifically in paediatric population with genu varus.
Another significant finding in this study is ICD has moderate correlation with cTFA and mTFA. There are several correlation studies that were reported on ICD. Saini et al found that a fair degree of correlation was established between ICD and tibiofemoral angle (TFA), measured clinically by a goniometer [8]. A similar finding between ICD and TFA was seen in other studies [6-11]. This suggested that both measurements can complement each other in monitoring genu varus. The importance of ICD measurement was highlighted by other authors. Cahuzac et al in 1995 has established a data for the normal values of varus profile of the legs in normal children between 10 and 16 years of age, whereby a measurement of ICD of more than 5 cm is considered abnormal [18]. This is supported by other investigators [14-19]. For younger children aged of at least 18 months, ICD of 4cm should be closely monitored [11].
The different degrees of correlation in various studies might be influenced by the different method of measurements. Mathew et al had found the clinical measurement of using ICD to have minimal intra-observer variability [6]. However, a standardized way of measurement and positioning of the patients is important to get a consistent finding. Obtaining a proper standing radiograph in a young child can proved to be challenging, so other measures such as footprint drawn on the floor have been suggested [11].
We also found that the difference of agreement between cTFA and mTFA measurement were significant. mTFA consistently produced a higher value with the mean difference around 5 degrees indicating that the angles were not similar between the two techniques. However, as mentioned earlier both measurements correlated with each other. This means that although not totally accurate as measured on radiograph (mTFA), clinical method can still show similar trend of deformity therefore useful for monitoring change or progress.
There were some limitations in our study. Firstly, our sample population was relatively small with a wide age range (1-17 years). Secondly, we only performed observer reliability study for the radiographic measurement. However, the clinical measurements were done by a single researcher, who was trained to perform the measurement following the standard protocol.
Conclusion
Clinical measurement of tibiofemoral angle and ICD to good correlation with radiological measurement, when performed with the child in standing position. Therefore, for monitoring purposes or serial alignment assessment, these methods are adequate.
Declarations
Conflicts of interest: The author(s) have no conflicts of interest to disclose.
Ethical approval: The study's ethical approval was obtained from the Universiti Kebangsaan Malaysia Institutional Ethical Committee (JEP-2020-194).
Patient consent (participation and publication): Verbal informed consent was obtained from patients for publication.
Source of Funding: Universiti Kebangsaan Malaysia
Role of Funder: The funder remained independent, refraining from involvement in data collection, analysis, or result formulation, ensuring unbiased research free from external influence.
Acknowledgements: None to be declared.
Authors' contributions: KJ and CYT conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript. CYT designed the data collection instruments, collected data and carried out the initial analyses. AFAR and AHAR coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Use of AI: AI was not used in the drafting of the manuscript, the production of graphical elements, or the collection and analysis of data.
Data availability statement: Note applicable.
