Phrenic Nerve Block for Management of Post-Thoracic Outlet Decompression Cough: A Case Report and Literature Review
Abstract
Introduction
Thoracic outlet syndrome is a group of disorders arising from compressive forces on the neurovascular bundle in that region due to different etiologies. This study aims to present a case with an intractable cough as a complication of the surgery and its management.
Case presentation
A 41-year-old woman had a 15-year history of bilateral upper limb pain and numbness. The pain worsened over the last two months. Tests and imaging confirmed thoracic outlet syndrome. Physiotherapy had no effect. She underwent thoracic outlet decompression (TOD) under general anesthesia via a supraclavicular incision. Post-surgery, she developed uncontrollable cough that didn't respond to medication. Two days after the operation, a bupivacaine (5%) injection near the phrenic nerve resolved the cough.
Literature review
The literature review identified several cases of TOD complications, including right phrenic nerve paralysis resolving in 3-6 months, unilateral right diaphragm dysfunction, and lung herniation successfully treated with thoracoscopic reduction. These cases underscore the diverse presentations and outcomes of TOD complications, highlighting the importance of early diagnosis and tailored management strategies.
Conclusion
A possible complication of surgical decompression for thoracic outlet syndrome is an intractable cough that can be relieved by the injection of local anesthesia into the area of the phrenic nerve.
Introduction
Thoracic outlet syndrome (TOS) encompasses a range of disorders that lead to the compression of the neurovascular bundle in the thoracic outlet [1,2]. It is commonly classified into three types: neurogenic TOS (nTOS), venous TOS (vTOS), and arterial TOS (aTOS) [3]. nTOS is the predominant type, representing more than 90% of the cases. TOS is more commonly seen in females and individuals who have poor muscle development, poor posture, or both. Determining the precise prevalence of TOS is challenging due to the non-specific nature of its symptoms. The estimated incidence of TOS ranges widely, with approximately 3 to 80 cases per 1000 people. TOS typically occurs in three distinct spaces: the scalene triangle, costoclavicular space, and subcoracoid space. This condition can arise due to congenital, acquired, or traumatic factors. Secondary causes include clavicular fracture and deficiency in the trapezius muscle, causing shoulder depression, further diminishing the thoracic outlet, and increasing pressure in the thoracic outlet [4]. After physical therapy as a conservative management, one of the management options for TOS is surgical decompression. The possible complications of such a procedure are numerous, including pneumothorax, hemothorax, chylothorax, bleeding, and nerve injuries such as brachial plexus, phrenic nerve, and thoracic nerve. Despite surgical intervention, the recurrence of symptoms, spanning from 15% to 30%, remains a notable consideration [5,6]. However, a severe cough has never been reported in the literature.
This study aims to report and discuss a case of a severe, intractable cough that developed after nTOS decompression and was managed by injection of local anesthesia. The references have been inspected for reliability, and the report has been written according to the CaReL guidelines [7,8].
Case Presentation
Patient information
A 41-year-old female presented with bilateral upper limb pain and numbness for 15 years, more pronouncedly on the right side. The pain progressed in the last two months.
Clinical findings
The provocative tests for TOS (scalenus muscle tenderness, elevation arm stress test, and Elvey test) were positive.
Diagnostic approach
Electromyography and nerve conduction studies showed nTOS, while chest X-rays, and cervical spine magnetic resonance imaging (MRI) were unremarkable. Doppler ultrasound of the right upper limb showed arterial and venous compression, suggesting nTOS.
Therapeutic intervention
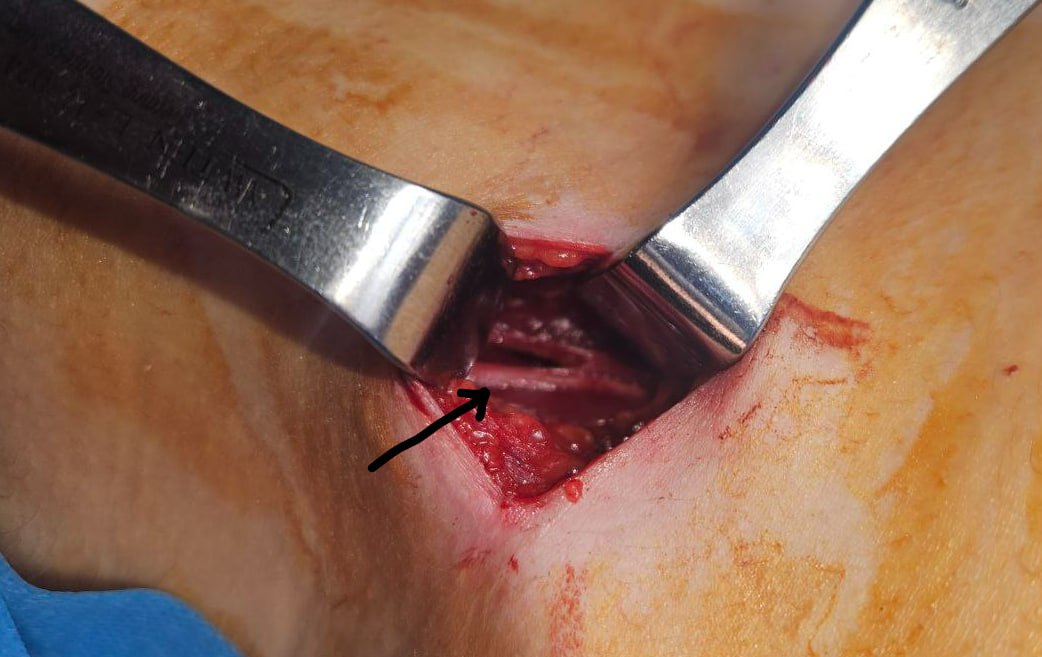
The patient was first advised to do physiotherapy before opting for more invasive interventions, but the patient’s symptoms did not improve after four weeks of physiotherapy. Consequently, the patient was prepared for thoracic outlet decompression (TOD). Under general anesthesia, in the supine position, through a 4-cm supraclavicular incision, anterior, middle, and posterior scalene muscles were resected. The first rib was isolated and resected. Neurolysis was done. The patient was extubated in the operating room. However, in the postoperative period, she developed a severe cough six hours after recovering from the anesthesia. The cough did not respond to the oral and intravenous medications. Two days after the operation, the patient was injected with 120 mg of bupivacaine (5%) into the area of the phrenic nerve in the supraclavicular region-site of the resected scalene anterior muscle [figure 1].
Follow-up and Outcome
The patient responded very well to the injection, and the cough disappeared.
Discussion
After reviewing the genuine literature, we identified several cases of TOD, including a 45-year-old male with right phrenic nerve paralysis post-operation resolving in 3-6 months, a 45-year-old female with postoperative unilateral right diaphragm dysfunction following TOD, and a 40-year-old female with lung herniation after thoracic outlet decompression surgery, which was successfully treated with thoracoscopic reduction and resection, showing no signs of recurrence after 9 months. These cases highlight the varied presentations and outcomes of TOD complications, ranging from respiratory issues to chronic pain, and emphasize the importance of early diagnosis and tailored management strategies [Table 1] [9-11].
|
Author (year)reference |
No. Case |
Age |
Gender |
Presentation |
Previous history |
Clinical examination |
Imaging findings |
Management |
Complication |
Outcome |
|
Heine et al. (1995) [9] |
1 |
45 |
Male |
Numbness and tingling in the right arm, shortness of breath post-operation |
Normal pulmonary reserve |
Post-operation: Dyspnea in the supine position, respiratory rate of 26 breaths per minute, decreased breath sounds in the right hemithorax |
Chest radiograph: Markedly elevated right hemidiaphragm. Fluoroscopic evaluation: Confirmed right phrenic nerve palsy with right diaphragmatic paralysis |
Initial: Restrict activities as tolerated. Follow-up: Continued elevation of the right hemidiaphragm at 3 months, normal pulmonary function tests in the seated position, moderate restrictive defect in the supine position. Six months post-operation: Asymptomatic, normal chest radiograph and fluoroscopic examination, normal pulmonary function tests in both seated and supine positions |
Right phrenic nerve paralysis leading to unilateral diaphragmatic paralysis |
Resolution of phrenic nerve paralysis within 3 to 6 months post-operation |
|
Cain et al. (2021) [10] |
1 |
45 |
Female |
Thoracic outlet syndrome |
Protein C deficiency, recent right thoracic outlet decompression surgery (3 weeks prior), left-sided thoracic outlet decompression surgery (7 months prior) |
dyspnea on exertion
|
Point-of-care ultrasound: decreased movement of right hemidiaphragm compared to left. CT angiography: marked right hemidiaphragm elevation with compressive atelectasis. Sniff test: abnormal motion of right hemidiaphragm during respiration and paradoxical movement during sniff.
|
Not mentioned |
Diagnosed with postoperative unilateral right diaphragm dysfunction.
|
Not mentioned
|
|
Su et al. (2012) [11] |
1 |
40 |
Female |
Chronic left shoulder pain, left upper extremity pain, paresthesias, numbness, decreased functional range of motion of the left shoulder, worsening of symptoms with arm elevation, dyspnea on exertion (4 years after thoracic outlet syndrom decompression)
|
Smoking, previous arthroscopic subacromial decompression and cervical discectomy and fusion, thoracic outlet decompression (supraclavicular approach) 4 years prior
|
Localizing tenderness over the left supraclavicular space, reproducible arm symptoms, visible bulge on the left side of the neck that increased with coughing and exhalation
|
CT scan: Herniation of a large emphysematous bulla from the apex of the left lung into the supraclavicular space, possible compression of the brachial plexus (size: 5.3 x 4.3 x 3.6 cm) |
Thoracoscopic reduction and resection of the herniated lung, pleural flap closure of the defect |
Lung herniation |
Discharged on postoperative day 2 with improvement on chest X-ray. No signs of lung herniation at 9 months follow-up, improvement of arm pain and dyspnea.
|
The shoulder structure predisposes the neurovascular bundle toward the upper limb to compressions during arm abduction at various levels of the thoracic outlet pathway. This neurovascular positional compression may cause pain, discomfort, or problems known as TOS. TOS is classed as a rare disease on both sides of the Atlantic ("NORD®" rare disease database/ORPHANET n°97330), with an estimated frequency of 2.5 to 4.0 cases per 100,000 people per year in the United States and 3 to 4 cases per 100,000 people per year in France. The high frequency of observations in athletes has prompted some scholars to believe that the prevalence of TOS may be significantly higher in these people [12]. In the current study, a 41-year-old female had been experiencing bilateral upper limb discomfort and numbness for 15 years, with more pronounced symptoms on the right side.
Clinical examination involves specific physical maneuvers to identify the type and cause of the syndrome. For nTOS, which is the most common form, physical exams include neck rotation and head tilting, which can elicit symptoms in the contralateral extremity, and the upper limb tension test (ULTT), which is comparable to the straight leg raising test for the lower extremity. Another important maneuver is abducting the arms to 90 degrees in external rotation (90° AER), which typically brings on symptoms within 60 seconds. Imaging studies are crucial for diagnosing TOS. X-rays can reveal cervical ribs or anomalous first ribs, often associated with aTOS. In the case of aTOS, X-rays almost always show these anatomical anomalies. For vTOS, which is indicated by arm swelling, cyanosis, and pain, ultrasound, and venography are used to detect subclavian vein obstruction. Arteriography is used in aTOS to visualize subclavian artery stenosis or aneurysms, often showing emboli arising from these lesions. MRI, or magnetic resonance angiography (MRA), can also be employed to visualize the compression of neurovascular structures [13]. In the current study, electromyography and nerve conduction studies showed nTOS, chest X-rays, and cervical spine MRI were unremarkable. Doppler ultrasound of the right upper limb showed arterial and venous compression, suggesting nTOS.
The initial management of nTOS is by physical therapy, usually for eight weeks. However, if the patient’s condition remains the same or has unsatisfactory improvement after physical therapy, a computed tomography (CT)-guided scalene muscle block can be attempted, which has an important diagnostic value due to its high specificity and sensitivity. Because if the patient's symptoms improve, it indicates that the patient has a high likelihood of benefiting from surgical intervention [14,15]. TOD is the surgical approach utilized for treating TOS. The aim of surgery in TOS is to relieve pressure on the neurovascular structures in the thoracic outlet via surgical decompression. TOD surgery involves the complete resection of the first rib (cartilage to cartilage), transection of the scalene muscles, and thorough neurolysis/venolysis or arteriolysis. Four distinct approaches are available for TOD surgery: transaxillary, supraclavicular, paraclavicular, and infraclavicular. While transaxillary, supraclavicular, and paraclavicular approaches apply to all forms of TOS, the paraclavicular approach is primarily employed in treating vTOS. The infraclavicular approach is not relevant for neurogenic or arterial TOS and is exclusively utilized for vTOS. Each approach has its advantages and limitations, and there is no consensus in the literature on the optimal approach. Therefore, the choice of the surgical approach for TOD should be based on the surgeon's preference and experience [16]. As in the current case, the patient was initially advised to undergo physiotherapy before proceeding with more intrusive measures, but her symptoms did not improve after four weeks of therapy. As a result, the patient was prepared for TOD.
Nonetheless, the surgery might result in various complications, ranging from temporary post-surgery discomfort to lasting disability. The complications vary, including persistent symptoms, injuries to the brachial plexus, phrenic nerve, and long thoracic nerve, leading to partial or temporary paralysis. Additionally, there is a risk of injuries to major blood vessels like the subclavian artery and vein, as well as axillary artery thrombosis. Other potential complications involve hemothorax, pneumothorax, and chylothorax [5]. This patient was free from the expected complications. However, she had a severe, intractable cough postoperatively. The presence of cough post-TODs is very rare, and there has been no other recorded case in the literature to date, at least to the best of our knowledge.
Scott R. Golarz and colleagues showed that supraclavicular decompression for nTOS often involves encountering variations in the anatomy of the phrenic nerve and brachial plexus more frequently. Surgeons operating within the thoracic aperture should have a good understanding of these variant anatomical structures to minimize the risk of nerve injuries, which can lead to severe postoperative complications [17]. A study by Katherine et al. showed that the brachial plexus, phrenic nerve, and long thoracic nerve are located in close proximity to the anterior and middle scalene muscles and the first rib, which are surgically removed to alleviate neurogenic, venous, and arterial thoracic outlet syndrome. Although nerve injury is a relatively rare occurrence, affecting approximately 1% of cases, it can result in significant complications such as hemidiaphragm paralysis, scapular winging, or motor and sensory deficits in the upper extremities. Considering the vital role of the upper extremity, nerve injury can have substantial negative impacts, highlighting the critical importance of understanding nerve anatomy and practicing careful surgical techniques during thoracic outlet syndrome procedures [18].
Phrenic nerve palsy or injury is linked to a reduced cough reflex, and considering the nerve block, the cough is not expected to occur. However, it is essential to note that the efficacy of bupivacaine is temporary, lasting less than 8 hours [19]. Between 40% and 76% of intubated patients experience coughing during the emergence from general anesthesia, and the physiological consequences of peri-extubation coughing can result in notable complications. These complications encompass neck hematoma following thyroidectomy or carotid endarterectomy, wound dehiscence after laparotomy, and intracerebral hemorrhage after intracranial surgery. To mitigate these risks, there is a consensus among authors for a "smooth emergence" strategy, aiming to minimize coughing and, consequently, prevent these potential complications [20]. The current case did not have any of the complications mentioned above. However, she presented with an intractable cough six hours after waking up from anesthesia that was unresponsive to medications. Fortunately, the patient responded well to the injection of local anesthesia into the area of the phrenic nerve. This may indicate neuropraxia (temporary nerve injury or irritation) rather than permanent nerve injury.
Conclusion
A possible complication of surgical decompression for TOS is an intractable cough that can be relieved by the injection of local anesthesia into the area of the phrenic nerve.
Declarations
Conflicts of interest: The author(s) have no conflicts of interest to disclose.
Ethical approval: Not applicable.
Patient consent (participation and publication): Written informed consent was obtained from the patient for publication.
Funding: The present study received no financial support.
Acknowledgements: None to be declared.
Authors' contributions: FHK was a significant contributor to the conception of the study and the literature search for related studies. SHM, RJR, SKA, PMK, MSM and AKG were involved in the literature review, the study's design, and the critical revision of the manuscript, and they participated in data collection. DSH, AAQ, and FA were involved in the literature review, study design, and manuscript writing. SSA, NSS, and FA Literature review, final approval of the manuscript, and processing of the tables. FHK and AKG confirm the authenticity of all the raw data. All authors approved the final version of the manuscript.
Use of AI: AI was not used in the drafting of the manuscript, the production of graphical elements, or the collection and analysis of data.
Data availability statement: Not applicable.
References
- Jones MR, Prabhakar A, Viswanath O, Urits I, Green JB, Kendrick JB, et al. Thoracic outlet syndrome: a comprehensive review of pathophysiology, diagnosis, and treatment. Pain and therap. 2019; 8:5-18. doi:10.1007/s40122-019-0124-2.
- Lukadi JL. Controversies in Thoracic Outlet Syndrome. Barw Med Jour. 2023;1(3):1. doi:10.58742/bmj.v1i2.40.
- Li N, Dierks G, Vervaeke HE, Jumonville A, Kaye AD, Myrcik D, et al., Thoracic outlet syndrome: a narrative review. Jour of Clin Med. 2021;10(5):962. doi:10.3390/jcm10050962.
- Abdalla BA, Kakamad FH, Namiq HS, Asaad SK, Abdullah AS, Mustafa AM, Ghafour AK, Kareem HO, Ahmed SQ, Mohammed BA, Hasan KM. Pediatric thoracic outlet syndrome: a systematic review with metadata. Ped Surg Inter. 2024;40(1):1-2 doi:10.1007/s00383-024-05769-y
- Hosseinian MA, Loron AG, Soleimanifard Y. Evaluation of complications after surgical treatment of thoracic outlet syndrome. Korean jour of thorac and cardiovasc surg. 2017;50(1):36. doi:10.5090%2Fkjtcs.2017.50.1.36.
- Atasoy E. Recurrent thoracic outlet syndrome. Hand Clin. 2004;20(1):99-105. doi:10.1016/s0749-0712(03)00085-4
- Abdullah HO, Abdalla BA, Kakamad FH, Ahmed JO, Baba HO, Hassan MN, et al. Predatory Publishing Lists: A Review on the Ongoing Battle Against Fraudulent Actions. Barw Med Jour. 2024;2(2):26-30. doi:10.58742/bmj.v2i2.91.
- Prasad S, Nassar M, Azzam AY, García-Muro-San José F, Jamee M, Sliman RK, et al. CaReL Guidelines: A Consensus-Based Guideline on Case Reports and Literature Review (CaReL). Barw Med Jour. 2024;2(2):13-19 doi:10.58742/bmj.v2i2.89.
- Heine MF, Asher EF, Roy TM, Ackerman III WE. Phrenic nerve injury following scalenectomy in a patient with thoracic outlet obstruction. Jour of Clin Anesth. 1995;7(1):75-9. doi:10.1016/0952-8180(94)00021-U.
- Cain W, Cai SS, Salcedo C, Embry S, Scalise M. Unilateral diaphragmatic dysfunction following thoracic outlet surgery diagnosed by point-of-care ultrasound. Jour Community Hosp Intern Med Perspect.2021;11(4):551-3. doi:10.1080/20009666.2021.1915550.
- Su F, Zoole JB, Thompson RW, Meyers BF, Kuo E. Lung herniation after supraclavicular thoracic outlet decompression. Ann Thorac Surg. 2012;93(5):1720-2. doi:10.1016/j.athoracsur.2011.08.059.
- Abraham P, Lecoq S, Mechenin M, Deveze E, Hersant J, Henni S. Role of Lifestyle in Thoracic Outlet Syndrome: A Narrative Review. Jour Clin Med. 2024;13(2):417. doi:10.3390/jcm13020417.
- Sanders RJ, Hammond SL, Rao NM. Diagnosis of thoracic outlet syndrome. Jour vasc surg. 2007;46(3):601-4. doi:10.1016/j.jvs.2007.04.050.
- Fugate MW, Rotellini-Coltvet L, Freischlag JA. Current management of thoracic outlet syndrome. Curr Treat Options Cardiovasc Med. 2009;11(2):176-83. doi:10.1007/s11936-009-0018-4.
- Laulan J, Fouquet B, Rodaix C, Jauffret P, Roquelaure Y, Descatha A. Thoracic outlet syndrome: definition, aetiological factors, diagnosis, management and occupational impact. Jour occup rehabil. 2011; 21:366-73. doi:10.1007/s10926-010-9278-9.
- Suzuki T, Kimura H, Matsumura N, Iwamoto T. Surgical approaches for thoracic outlet syndrome: a review of the literature. Jour Hand Surg Glob Online. 2023;5(4):577-84. doi:10.1016/j.jhsg.2022.04.007
- Golarz SR, White JM. Anatomic variation of the phrenic nerve and brachial plexus encountered during 100 supraclavicular decompressions for neurogenic thoracic outlet syndrome with associated postoperative neurologic complications. Ann Vasc Surg. 2020; 62:70-5. doi:10.1016/j.avsg.2019.04.010.
- Giuliano K, Lum YW. Management of nerve dysfunction after first rib resection. Thorac Out Synd. 2021:435-40. doi:10.1007/978-3-030-55073-8_47.
- Steverink JG, Piluso S, Malda J, Verlaan JJ. Comparison of in vitro and in vivo Toxicity of Bupivacaine in Musculoskeletal Applications. Front Pain Res. 2021; 2:723883. doi:10.3389/fpain.2021.723883.
- Tung A, Fergusson NA, Ng N, Hu V, Dormuth C, Griesdale DE. Medications to reduce emergence coughing after general anaesthesia with tracheal intubation: a systematic review and network meta-analysis. Br Jour Anaesth. 2020;124(4):480-95. doi:10.1016/j.bja.2019.12.041.

This work is licensed under a Creative Commons Attribution 4.0 International License.

